Overview
Occupational therapists provide diverse expertise to primary care teams helping patients get fast access to the right care. Using health population approaches, they offer bespoke services for specific patient groups. Their interventions are proactive and preventative to keep patients functioning and active. Occupational therapists can help target the biggest causes of reduced life expectancy. They are clinically trained to work holistically across the life span for patients with physical, mental and social needs. (RCOT, 2024).
Scope of Practice
Role Responsibilities
They can work across the life span with patients with heart disease, COPD, stroke, diabetes, dementia, mental illness, rheumatoid and osteoarthritis, cancer, learning disabilities, palliative care, obesity and smoking.
- Occupational therapists carry out physical and psychosocial assessments that consider health and home management, education, work, leisure, and social participation.
- They formulate plans for therapy including differential diagnosis of conditions impacting on health, functional ability, and activity levels.
- They proactively work in partnership with patients to find solutions that improve health and activity levels.
- Occupational therapy interventions are practical, realistic and goal orientated. They adapt activities to help patients stay active in their everyday lives.
These are several key patients that can be directly triaged to First Contact Occupational Therapists, without having to see a GP first:
- Adults with mental health problems
- Older adults with frailty related problems
- Working age adults requesting fit notes
What occupational therapists offer – RCOT
Entry Requirements
- BSc in or pre-reg MSc in Occupational Therapy
- 3 – 5 years post graduate
- Registered member of the Health and Care Professionals Council (HCPC)
- Able to operate at an advanced level of practice
Training and Development
Mandatory Training
See above ‘Entry Requirements’
Standard Training (on entry to Primary Care)
First Contact Practitioner (FCP) Recognition
FCP roles began with the development of the FCP Physiotherapist in 2014, in response to the shortage of GPs in Primary Care. FCP roles are designed to support GPs as part of an integrated care team and to optimise the patient care pathway by seeing the right person in the right place at the right time.
To create sustainability for multi-professional FCP roles, there is a need to build a clear national Primary Care training pathway for clinicians moving into FCP roles and then onto Advanced Practitioner roles. Therefore the NHSE ‘Roadmaps to Practice’ were published to support educational pathways for clinicians.
Please find below links to the Roadmap to Practice which will help service providers, managers and Occupational Therapists themselves to identify what training, qualifications and competencies they should have to safely and effectively practice at first contact practitioner levels.
Working alongside the ‘First Contact Practitioners AND Advanced Practitioners in Primary care (Occupational Therapist); Roadmap to practice (link above), FCPs must have completed both stage 1 and Stage 2 of the Roadmap to gain recognised First Contact Practitioner MSK status.
- The OT can be seen as a ‘trainee FCP’ until full FCP recognition is gained.
- At present there are 2 main educational pathways by which one can train to be a Occupational Therapist:
- Via an FCP portfolio completely.
- Via portfolio with taught routes via HEI’s. (This may include supported portfolio option, where HEI supports clinician with portfolio completion)
There are two stages to First Contact Practitioner recognition:
- Stage 1: Preferably, must be completed with a portfolio of evidence and verified before employment in Primary Care. The KSA must be completed prior to employment as a FCP or AP in Primary Care to assure patient safety. For clinicians already working in primary care this can be completed retrospectively
- Stage 2: Is completed with a portfolio of evidence, including formal module completion and is verified in Primary Care. This is the recognition process of the application of the KSA in Stage 1 to clinical practice in Primary Care. Best practice is that this should be completed within 6 – 12 months for a full-time member of staff but this can be longer provided a completion date is agreed with the employer.
- ‘Trainee’ FCP’s are advised to keep a folder of evidence ready to submit in the final stages of their pathway.
Education providers
There are education providers across the UK that are successfully running MSK FCP taught modules. NHSE has also provided funding support for applicants to attend these modules. All the providers have committed to taking learners from outside the region that they are based.
Please see information and links below to each provider for further information. If you are looking to enquire about an FCP taught module, please contact the education provider directly to discuss your individual requirements.
Additional Training
- Advanced Practice Recognition – Please see link to the SNEE TH Advanced Practice page for full information on Advanced Practice
Supervision Requirements
Supervision is a process of professional learning and development that enables individuals to reflect on and develop their knowledge, skills and competence, through regular support from another professional.
Supervision can have different forms and functions and a number of terms are used to describe these. For this guidance we use the below terms and define them as follows:
- Clinic/practice supervision: day-to-day support provided by a named/duty senior/more experienced clinician for issues arising in the practice.
- Clinical/professional supervision: regular support from a named senior/experienced clinician/practitioner to promote high clinical standards and develop professional expertise.
- Educational supervision: supports learning and enables learners to achieve proficiency.
It is recommended that Occupational Therapists have access to appropriate clinical supervision and an appropriate named individual in the PCN to provide general advice and support on a day-to-day basis. This would typically be more senior/experienced OT, recognised Advanced Practitioner or may also be another registered health care professional as appropriate i.e. GP, consultant practitioner. Recommended minimum frequency of a 1 hour supervision meeting is monthly. Whilst an FCP trainee, it is recommended that daily debriefs/reflection time is also supported.
Supervision Guidance for primary care network multidisciplinary teams (NHSE, 2023)
Clinical and Education supervisors have an integral role to support learners through the FCP Recognition process and to provide assurance that the practitioner has demonstrated the knowledge, skills and attributes required to work in a FCP role in primary care. One of their key roles is to review a learner’s portfolio of evidence and decide whether the individual has met the requirements of an appropriate FCP Roadmap.
For both the FCP Supported Portfolio and FCP Taught routes, Clinical and Education supervisors will work with an education provider, as part of the institution’s quality assurance processes, to support the learner to meet the appropriate level 7 learning outcomes of the applicable FCP Roadmap. Supervisors will sign-off the portfolio of evidence on successful completion.
The route to becoming a supervisor for FCP recognition and training has recently been updated. Please see the NHSE ‘First Contact Practice FAQ’s’ page for the latest updates on the process. For further information regarding the FCP Roadmap pathway and processes, please visit: Roadmaps to Practice | Health Education England (hee.nhs.uk)
Funding
AFC Band 7/8a
100% of actual salary plus defined on costs covered via ARRS Scheme.
Training and development funding
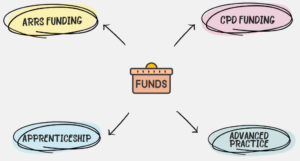
Occupational therapists may be entitled to wider NHSE commissioned funding to support their training and development requirements. Please contact the training hub for more information on this.
Recruitment Information
Where a PCN employs or engages a Occupational Therapist under the Additional Roles Reimbursement Scheme, the PCN must ensure that the Occupational Therapist meets the ‘Minimum Role Requirements’ stipulated in Annex B of the Network DES
Please find various resources in this section to assist in the recruitment and embedding of the Occupational Therapist role in General Practice.
